Cardiovascular Topics
Gender inequality in hypertension
Why cardiovascular disease (CVD) kills more women than men, and what can be done about it.

CVD leading cause of death in women
'"Cardiovascular disease is the leading cause of death in women. Many CVD risk factors in women are still under-recognized and under-treated. Hypertension can cause a variety of symptoms that are often attributed to menopause. Therefore it is important for (young) women to be involved in their own treatment such as by monitoring their blood pressure at home"
Angela H.E.M Maas, MD PhD FESC
Professor in Women's Cardiac Health
Radboud University Medical Center
Why cardiovascular disease (CVD) kills more women than men, and what can be done about it1
CVD is the leading cause of death globally. It takes approximately 17.9m lives every single year; through coronary heart disease, cerebrovascular disease, rheumatic heart disease and other conditions that attack the heart and blood vessels. With more than 4 out of 5 CVD deaths being the result of heart attacks and strokes, and a third of these deaths occurring prematurely in people under 70 years old.2
However, it’s also true that CVD does not treat the sexes equally. Because CVD takes away more female lives than male. Even in women under 65 years of age, where over double the number of women die from CVD than they do from breast cancer. Unlike cancer, where mortality for some cancers in women is on the decline, death rates for cardiovascular diseases is stagnating or has increased. With more and more women having to live with chronic incurable diseases of the heart and vascular system. So, it’s imperative that awareness is raised amongst healthcare professionals and women of all ages.1
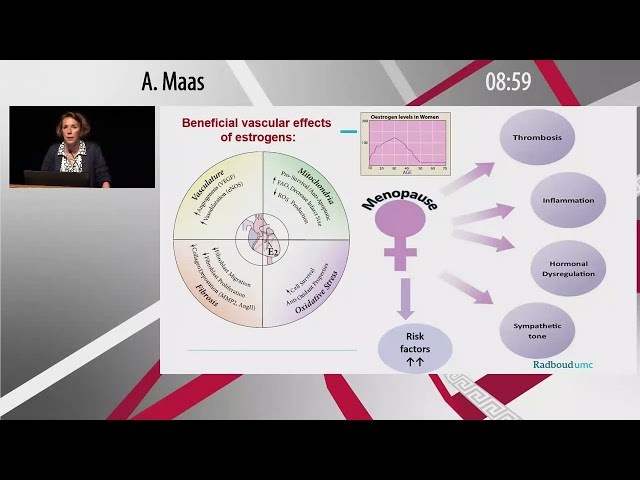
Furthermore, hypertension is recognised as one of the key risk factors for CVD partly because of the damage it can do to blood vessels and the circulatory system. Although today it’s well established that men have a higher prevalence for hypertension; this is prior to the onset of menopause in women.3
Following menopause, women can show a rapid and distinct increase in the prevalence of hypertension in comparison to men, to the point where prevalence exceeds that of men.3
There are other gender-specific risk factors for women to develop CVD, including the following:4
Gestational diabetes
Hypertensive disorders due to pregnancy
Premature menopause
Preterm delivery
Polycystic ovary syndrome
Systemic inflammatory and autoimmune disorders
Plus, there is evidence to suggest that women, primarily due to inequalities in gender, are at further risk from other under-recognised factors, including psychosocial, domestic abuse, socioeconomic deprivation, poor health literacy and environmental risk factors4

Indeed, it’s also interesting to note that women have historically been under-represented (or even excluded) in cardiovascular clinical trials. Consequently, due to a lack of clinical data, we are not really aware if hypertension should be managed differently in women than in men; this includes treatment goals and choice and dosages of antihypertensive medication.5
No doubt, this has led to missed opportunities to gain knowledge on differences between the genders when responding to CVD treatments, which could well have an impact on optimising clinical outcomes for women. For example, the risk for CVD increases at a lower BP level for women (in comparison to men), which suggests a gender specific threshold for diagnosis of hypertension could be reasonable.4
Moreover, with hypertension in women often being misdiagnosed or mislabelled as ‘stress’ or ‘menopausal symptoms’, which if left untreated could put more women at risk of atrial fibrillation (AF), heart attacks, stroke and other CVDs. What can be done to provide women with greater levels of safeguarding against hypertension and consequently CVD? While greater awareness of the risks is crucial, the following points could also help:6
Closer collaboration between cardiologists, gynaecologists and endocrinologists
Women raising previous medical events with their doctors, such as complicated pregnancies and early menopause
Women home-monitoring and tracking their blood pressure and sharing results with their doctor
E-learning: Hypertension in Women
If you would like to discover more about hypertension in women (and how it differs from men) please visit our OMRON Academy module on the subject, which you will find here.
(Nighttime) hypertension in Women
Prof. Angela Maas, Nijmegen, The Nehterlands
References
1: European Society of Cardiology. The ESC. Advocacy. Available at: https://www.escardio.org/The-ESC/Advocacy/women-and-cardiovascular-disease. Accessed December 2022.
2: World Health Organization. Health Topics. Cardiovascular diseases. Available at: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1. Accessed February 2023.
3: Ramirez, L.A. and Sullivan, J.C. (2018). Sex Differences in Hypertension: Where We Have Been and Where We Are Going. American Journal of Hypertension, [online] 31(12), pp.1247–1254. doi:10.1093/ajh/hpy148.
4: The Lancet. Infographics. Women and cardiovascular disease. Available at: https://www.thelancet.com/infographics-do/women-and-cardiovascular-disease. Accessed December 2022.
5: Gerdts, E., Sudano, I., Brouwers, S., et al. (2022). Sex differences in arterial hypertension. European Heart Journal, [online] 43(46), pp.4777–4788. doi:10.1093/eurheartj/ehac470.
6: The University of British Columbia. Women’s Health Research Centre. Women’s Health Blog. Available at: https://womenshealthresearch.ubc.ca/blog/high-blood-pressure-misunderstood-women-and-not-just-men. Accessed December 2022.
